Trauma Informed Practice Course
The Competence and Confidence to Work with Trauma in Your Practice.
The following article is taken from our Trauma-Informed Practice course.

The Competence and Confidence to Work with Trauma in Your Practice.
Trauma often lurks beneath the surface, manifesting in ways that clients may not immediately recognise or disclose. As therapists, it is essential to develop the skill of listening for clues that might indicate the presence of trauma. This practice does not involve diagnosing trauma but instead being attuned to the subtle signs and symptoms that suggest a traumatic history.

Listening for Clues in Trauma-Informed Practice
Clients may not always present trauma as their primary issue. Instead, they might seek therapy for related symptoms such as anxiety, depression, or chronic pain. However, careful listening can reveal underlying trauma. Clients might describe experiences or symptoms that, while not overtly labelled as trauma, suggest its presence.
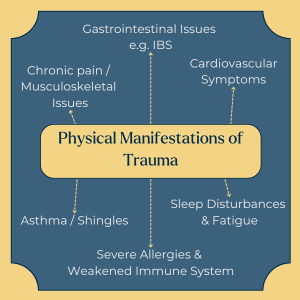
Trauma can manifest physically in various ways that may be overlooked if not carefully considered. For example, clients might report chronic pain conditions like fibromyalgia or persistent headaches without linking these symptoms to past traumatic events. Lower back pain and other musculoskeletal issues are also common, often dismissed as purely physical ailments. However, they might have a deeper psychological origin related to trauma.
Furthermore, gastrointestinal issues such as irritable bowel syndrome (IBS) might be a sign of unresolved trauma, mainly if these symptoms appear or worsen during periods of emotional distress. Cardiovascular symptoms, including unexplained chest pains and heart palpitations, can also be linked to trauma, especially in clients who have experienced acute stress or panic attacks.
Trauma stress weakens the immune system, making the body more susceptible to various conditions. Asthma, shingles, and even severe allergies may flare up under stress, which can be indicative of the body’s response to unresolved trauma. Sleep disturbances and fatigue are other critical indicators. A client who struggles with insomnia or who reports constant tiredness despite sufficient rest might be dealing with the aftereffects of trauma. These physical symptoms are not just isolated complaints but can be seen as the body manifesting the distress the mind struggles to process.
As counsellors, it is vital to listen attentively to these complaints and consider them within the broader context of the client’s life and experiences. Encouraging clients to connect their physical symptoms to their emotional and psychological states can be a significant step toward healing.
Cognitive and psychological impairments following trauma can be as debilitating as physical symptoms. Clients may exhibit significant decision-making difficulties, feeling overwhelmed by choices or avoiding decisions altogether. This can be due to a lack of confidence or pervasive anxiety.This difficulty can stem from a disrupted sense of agency, a common aftereffect of trauma where clients no longer trust their judgement.
Another key symptom is a lack of motivation. A client may express a pervasive sense of apathy or be unable to engage in activities they once enjoyed. This can be a direct result of trauma, where the emotional energy required to cope with daily life is drained, leaving the individual feeling depleted and unmotivated.
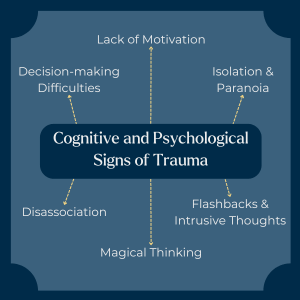
Isolation and paranoia can also be prominent. A client might withdraw from social interactions or become overly suspicious of others. These behaviours are often rooted in past experiences where trust was broken. Disassociation is another critical symptom, where clients might describe feeling disconnected from reality or their own emotions and body. This can be a coping mechanism developed during traumatic experiences, where disassociation serves as a way to protect themselves from overwhelming emotions.
Magical thinking—where a client might deny or rationalise abusive behaviour by an abuser—can complicate the therapeutic process. For instance, a client might reinterpret their traumatic experiences to minimise the abuser’s actions or to maintain a sense of control. Addressing these thought patterns with sensitivity and care is crucial to helping the client move toward a more accurate understanding of their experiences.

Flashbacks and intrusive thoughts are among the more distressing symptoms of trauma. Clients may suddenly relive traumatic events or be haunted by persistent, unwanted thoughts that disrupt their daily lives. These symptoms can be particularly challenging to manage, as they often feel uncontrollable to the client.
In therapy, gently exploring these cognitive and psychological signs can help clients make connections between their symptoms and past experiences. This process not only validates their feelings but also provides a framework for understanding and eventually healing from their trauma.
In the therapy room, it’s crucial to remain aware of the subtle signs that may indicate trauma in your clients. While therapists are not responsible for diagnosing trauma, we can benefit from reflecting on the physical and cognitive symptoms clients present, which might suggest underlying trauma.
Additionally, discussing these observations with peers and supervisors can provide valuable insights and support. By integrating current trauma research with your clinical observations, you can enhance your ability to respond effectively to the complex needs of clients affected by trauma.
Listening for Clues in Trauma-Informed Practice
While a client may present with symptoms like anxiety, depression or chronic pain, a counsellor can attune to more subtle indicators – for example physical complaints (e.g. chronic pain, gastrointestinal upset, sleep problems), cognitive difficulties (such as indecision, lack of motivation), dissociation, intrusive thoughts or withdrawal – and gently explore whether trauma might be underpinning them.
Common physical manifestations include musculoskeletal and chronic pain, headaches, gastrointestinal issues (e.g. IBS), cardiovascular symptoms, sleep disturbances, fatigue, weakened immunity, and stress‑triggered conditions like asthma or shingles.
Therapists can reflect on client symptoms, discuss observations in supervision or peer consultation, integrate trauma research with clinical insight, and sensitively bring up the possibility of past trauma without attempting to diagnose – thereby supporting deeper understanding and therapeutic alliance.
Listening for clues is an essential skill in trauma-informed practice. By being attuned to the signs of trauma, counsellors and psychotherapists can provide more empathetic and effective support. This approach enhances the therapeutic relationship and empowers clients to understand and address the root causes of their symptoms.
Peres, J., Gonçalves, A., & Peres, M. (2009). Psychological trauma in chronic pain: Implications of PTSD for fibromyalgia and headache disorders. Current Pain and Headache Reports, 13(5), 351. Available at: Academia.edu
Counselling Tutor provides trusted resources for counselling students and qualified practitioners. Our expert-led articles, study guides, and CPD resources are designed to support your growth, confidence, and professional development.
👉 Meet the team behind Counselling Tutor
Notice any broken link or issues with this resource? Kindly let us know by email
Email us