Trauma Informed Practice Course
The Competence and Confidence to Work with Trauma in Your Practice.
The following article is taken from our Trauma-Informed Practice course.

The Competence and Confidence to Work with Trauma in Your Practice.
The relationship between trauma and physical health is profound and multifaceted, presenting unique challenges for counsellors and psychotherapists. This article explores how trauma affects body function, both during and long after the traumatic event, and provides insights into how these physiological changes manifest in clients. The discussion is anchored in key concepts from The Body Keeps the Score by Bessel van der Kolk and other influential sources.
By the end of this article, you will:
Body Function and Trauma
Trauma, particularly severe forms such as PTSD, affects the entire human organism—body, mind, and brain. According to van der Kolk, the body often continues to defend against a threat long after it has passed, maintaining a state of heightened stress mobilization. This prolonged state can lead to a range of physical health issues that therapists must be mindful of when working with clients.
A common characteristic of trauma, particularly dissociation, is the non-verbalisation of feelings, also known as alexithymia. This condition involves a lack of words for emotions and often directs the individual’s focus away from people towards things, manifesting in behaviours such as selective mutism. Alexithymia can also be experienced by individuals with autism, and isn’t always a result of trauma.
A powerful example of alexithymia as a response to trauma is illustrated in the story of author and civil rights activist Maya Angelou, who lost her voice for almost five years following the trauma of sexual abuse. This type of response highlights how deeply trauma can impact a person’s ability to express themselves verbally, making it crucial for practitioners to recognise and address non-verbal signs of trauma.
One of the key physiological responses to trauma is the increase in cortisol levels, a stress hormone that prepares the body for battle by boosting blood sugar levels and tissue repair mechanisms. While this response is beneficial in the short term, chronic elevation of cortisol can lead to significant health problems, including depression, heart disease, and other stress-related illnesses.
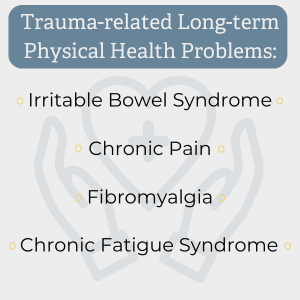
Trauma survivors are notably more prone to long-term physical health problems such as irritable bowel syndrome, chronic pain, fibromyalgia, and chronic fatigue syndrome. For therapists, it is important to consider these physical symptoms as potential indicators of unresolved trauma rather than viewing them as purely medical issues.
Substance misuse is another common issue among trauma survivors. As noted by Gabor Maté, drugs can make the pain tolerable, offering a temporary escape from the distressing memories associated with trauma. In cases of severe addiction, such as heroin use, there is often a history of traumatic events, with the substance acting as an analgesic for both physical and emotional pain.
Counsellors need to be aware of the strong connection between trauma and substance misuse, recognising that addiction may be a coping mechanism rather than the primary issue. Addressing the underlying trauma can be key to successful recovery.
An essential aspect of trauma-informed therapy is the integration of both psychological and physiological approaches. Recognising that trauma affects the whole person—mind, body, and brain—allows therapists to provide more holistic care. This approach may involve addressing the client’s physical symptoms and emotional experiences, helping them achieve a state of equilibrium where the body no longer feels threatened.
When working with trauma survivors, it is crucial to acknowledge the physical burden they may carry alongside the psychological effects. This involves recognising symptoms like chronic pain or gastrointestinal issues as potential remnants of trauma rather than isolated medical conditions. By considering the client’s overall health and encouraging discussions around physical symptoms, you can better understand the full impact of trauma and provide more effective support.
Body Function and Trauma
A: Trauma can keep the body in a heightened stress response, with chronically elevated cortisol leading to issues like chronic pain, IBS, fibromyalgia, fatigue, depression, and heart disease.
A: Trauma can cause alexithymia – a difficulty in identifying or verbalising feelings – which may lead to behaviours such as selectively muting one’s voice and turning away from emotional connection.
A: Counsellors should see symptoms like chronic pain or substance misuse as possible trauma responses, integrating attention to body and mind to support clients toward equilibrium.
Understanding the intricate link between body function and trauma is vital for counsellors and psychotherapists. By adopting a holistic approach that considers both the mind and body, you can more effectively address the lasting impacts of trauma. Recognising physical symptoms as part of the trauma response and not merely as separate medical issues will enable you to support your clients more comprehensively on the path to healing.
van der Kolk, B. (2015). The Body Keeps the Score. UK: Penguin Books.
Maté, G. (2008). In the Realm of Hungry Ghosts. London: Ebury Publishing.
Sanderson, C. (1990). Counselling Adult Survivors of Child Sexual Abuse. London: Jessica Kingsley Publishers.
Richmond, C. (2022). Emotional Trauma and the Mind-Body Connection. WebMD. Available at: WebMD.
These resources provide additional insights into the complex relationship between trauma and the body, offering valuable perspectives for therapists seeking to deepen their understanding and enhance their practice.
Counselling Tutor provides trusted resources for counselling students and qualified practitioners. Our expert-led articles, study guides, and CPD resources are designed to support your growth, confidence, and professional development.
👉 Meet the team behind Counselling Tutor
Notice any broken link or issues with this resource? Kindly let us know by email
Email us