Trauma Informed Practice Course
The Competence and Confidence to Work with Trauma in Your Practice.
The following article is taken from our Trauma-Informed Practice course.

The Competence and Confidence to Work with Trauma in Your Practice.
Understanding and avoiding retraumatisation is crucial for counsellors and psychotherapists, as it directly impacts the efficacy of therapeutic interventions. This article explores practical strategies and critical considerations for avoiding retraumatisation, ensuring that therapy remains a safe and supportive process for clients who have experienced trauma.
Retraumatisation not only disrupts the healing process but can also lead to setbacks in therapy, prolonging the recovery journey for clients. By understanding the nuances of trauma responses and implementing specific strategies, you can create a safer therapeutic environment that promotes trust and recovery.

Avoiding Retraumatisation: Essential Strategies for Therapists
By the end of this article, you will be able to:
Retraumatisation occurs when a client is exposed to stimuli that trigger memories of a traumatic event, leading them to relive the trauma within the therapeutic setting. This can severely undermine the therapeutic process, eroding the client’s trust in the therapist and, by extension, in therapy itself. Therefore, it is imperative that you actively work to avoid situations that could retraumatise your clients.
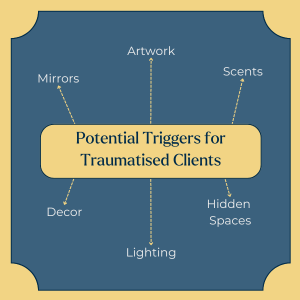
Triggers are stimuli that can evoke a traumatic response in clients. These can range from specific smells or sounds, to visual cues like mirrors and the therapist’s appearance. For example, one client expressed discomfort with mirrors, leading to covering all mirrors in the therapy room. This demonstrates the importance of attuning to the client’s needs and creating a physically and emotionally safe environment.
A practical approach to preventing triggers includes having an up-to-date picture of yourself on your website. This helps clients feel more secure, knowing what to expect when they meet their therapist. In one instance, a therapist updated their profile picture after growing a beard to ensure that the image matched their current appearance, thus avoiding any unexpected reactions from clients.
Assessment tools like CORE-10 are invaluable in trauma-informed practice. These tools enable clients to communicate their experiences and emotions without verbalising potentially distressing details. The CORE-10, for instance, allows you to gain insight into the client’s condition through a series of questions, helping you identify issues such as anxiety or sleeplessness, which are common in trauma survivors.
Using such tools, practitioners can better understand the client’s experiences and adjust their therapeutic approach accordingly, making it less likely for clients to become retraumatised during sessions.
Pre-planning involves careful consideration of the therapeutic environment and the therapist’s approach to sessions. For instance, therapists should be mindful of the smells in the therapy room, as certain scents can trigger traumatic memories. If a client is sensitive to a particular smell, it is crucial to eliminate that scent from the environment or, if unavoidable, inform the client in advance.
Moreover, therapists should ensure that the therapy room is free of any potential triggers, such as curtained-off areas, which may cause anxiety or suspicion in clients with trauma histories. In one example, a client initially wary of hidden spaces in the room eventually felt secure enough to ignore them as therapy progressed, illustrating the effectiveness of a thoughtful and responsive approach.
Traumatised clients often need to control the flow of information they share during therapy. This is partly because revisiting traumatic events can be overwhelming, and clients may fear judgement or upsetting the therapist. A key aspect of trauma-informed care is respecting the client’s boundaries and allowing them to disclose their experiences at their own pace. This patient, non-judgemental approach helps build trust and encourages clients to open up when ready.
Therapists should also be aware of trauma bonding, where clients may have complex emotional ties to their abusers. Understanding this dynamic is crucial in maintaining a supportive and non-judgemental therapeutic environment.
Avoiding Retraumatisation: Essential Strategies for Therapists
Allowing clients to set the speed and depth of disclosure – especially around traumatic events – helps them feel in control and prevents overwhelming them. Therapists monitor non‑verbal cues and use reflective listening to ensure safety and emotional comfort.
Therapists can avoid triggering clients by anticipating potential distress points, like room layout or hidden spaces, and thoughtfully planning sessions using outcome tools such as the CORE‑10 to assess emotional readiness.
Resisting retraumatisation ensures therapy supports healing rather than harm. Grounded in trauma‑informed care, this protective approach is central to creating trust, safeguarding clients’ well‑being, and nurturing a therapeutic relationship that fosters recovery.
Avoiding retraumatisation is an essential component of trauma-informed practice. By understanding potential triggers, using assessment tools like CORE-10, pre-planning the therapeutic environment, and working at the client’s pace, therapists can significantly reduce the risk of retraumatisation. These strategies safeguard the client’s well-being and strengthen the therapeutic relationship, fostering a safe and effective healing process.
Adopting trauma-informed practices is essential for safeguarding clients from retraumatisation. These strategies protect the client’s well-being and promote more effective and meaningful therapeutic outcomes.
CORE IMS. (2022). CORE Outcome Measurement Tools. Available online.
Counselling Tutor provides trusted resources for counselling students and qualified practitioners. Our expert-led articles, study guides, and CPD resources are designed to support your growth, confidence, and professional development.
👉 Meet the team behind Counselling Tutor
Notice any broken link or issues with this resource? Kindly let us know by email
Email us